 1. What is a traumatic brain injury?
1. What is a traumatic brain injury?
If you experience any forceful contact to your head, and it disrupts your brain’s natural functions, then you’ve experienced a traumatic brain injury, or TBI. Your brain can be injured by other conditions, like infections or strokes, but those kinds of injuries are called acquired brain injuries, or ABIs. They can be just as life altering as a TBI.
Doctors classify TBIs as either mild, moderate, or severe. Since most TBIs are mild, many people who sustain a TBI find that their symptoms get better over time. In fewer but more serious cases of TBI, the effects of the damage can last a lifetime.
2. How many people have TBI?
It’s hard to imagine, but almost 1.7 million Americans sustain a TBI each year. Most people who are treated at an emergency room are released, but approximately 275,000 are admitted annually into the hospital. Additionally, each year, more than 52,000 die as a result of the TBI, and some 125,000 are permanently disabled as a result of the injury.
Although we don’t know the number of people with TBI who aren’t seen in an emergency department, the Centers for Disease Control and Prevention estimates that at least 3.2 million Americans are permanently disabled as a result of a TBI.
 3. What causes TBI?
3. What causes TBI?
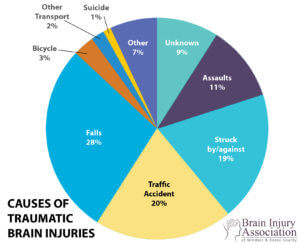
The leading causes of TBI are:
Falls (35.2%);
Motor vehicle/traffic crashes (17.3%);
Struck by/against (16.5%);
Assaults (11%);
Unknown/other (21%)1
Blasts are a leading cause of TBI for active duty military personnel in war zones.
4. Who is at highest risk for TBI?
Males are approximately 1.5 times as likely as females to sustain a TBI.
The age groups at highest risk for TBI are 0 to 4 year olds, 15 to 19 year olds, and adults aged 65 years and older.
Certain military duties increase the risk of sustaining a TBI.
African-Americans have the highest death rate from TBI.
5. What are the costs of TBI?
TBI takes a big toll on the American economy in 2000, it cost the US approximately $60 billion dollars overall.
The more severe the injury is, the more expensive it is to treat. If you were to experience a severe brain injury today, it would cost anywhere from $600,000 to $1.8 million dollars to care for you over your lifetime. If you’re a veteran, that cost could be much higher, since wartime TBIs are often accompanied by other injuries as well.
6. How does a TBI affect the brain and body?
When a TBI occurs, anything having to do with your brain is potentially affected. That means your basic body functions, like eating and sleeping, can be altered. It also means that the complex parts of your life, your emotions, your thoughts, and your ability to communicate can also be disrupted.
In serious cases, TBI can also affect the brain’s electrical system, causing seizures. Such a condition is commonly known as epilepsy. TBI is also known to increase the risk for other conditions such as Alzheimer’s and Parkinson disease.
 7. What are some common obstacles that arise after a TBI?
7. What are some common obstacles that arise after a TBI?
Treating TBI isn’t simple, and that creates many challenges for people with TBI and their families. In a 2006 report, the Institute of Medicine recognized the hardships that TBI creates and issued a report saying:
Many people with TBI experience persistent, lifelong disabilities. For these individuals and their caregivers, finding needed services is, far too often, an overwhelming logistical, financial, and psychological challenge. Individuals with TBI-related disabilities, their family members, and caregivers report substantial problems in getting basic services, including housing, vocational services, neurobehavioral services, transportation, and respite for caregivers. Yet efforts to address these issues are stymied by inadequate data systems, insufficient resources, and lack of coordination. TBI services are rarely coordinated across programs except in some service sites. Furthermore, in most states, there is no single entry point into TBI systems of care.”
Even long after an injury has happened, many people find that they require certain things that aren’t readily available. The most frequent unmet needs are:
Improving memory and problem solving;
Managing stress and emotional upsets;
Controlling one’s temper; and
Improving one’s job skills.
8. What are some long-term effects of TBI?
Because the human brain is so complicated, it’s extremely difficult to predict the long-term effects of any TBI. Most cases of mild TBI will resolve over a course of time with minimal problems. In the case of more serious TBIs, a person can experience any number of changes over the course of months and years.
Many people with TBI have problems with basic cognitive skills. It’s hard for them to pay attention or concentrate, and they might have trouble learning new material. A TBI can also make you think more slowly, or cause you to get easily confused. Even insight, the ability to clearly perceive a situation, can be affected. People with TBI may become impulsive, or develop unusual habits. Things that were once easy, like talking and listening, may become difficult or impossible.
Because the brain regulates our emotional and psychological lives, TBI can substantially alter your sense of mental wellness. The TBI might cause a personality change, or introduce mental problems. A person with TBI may have mood swings, depression, irritability, aggression, or disinhibition.
Vision problems are a common side effect of TBI, as are changes in your other senses: smell, taste, touch, and hearing. Problems with balance, vertigo, and ringing in the ears are also common. In a small percentage of cases, seizures occur as a result of TBI and may involve a loss of consciousness and muscle contractions. In many cases, anticonvulsive drugs or surgical intervention may help to prevent or slow seizure activity.
In severe cases that affect the brain’s most basic functions, fundamental abilities can be altered or inhibited. Paralysis or spasticity (muscle tightening) can affect a person’s ability to move, swallow, or breathe. Digestive problems can arise, and hormonal changes may result. Women with TBI often experience menstrual difficulties.
With appropriate help, however, a person with TBI can find ways to cope with these difficulties.
 9. What thought-related changes may occur due to a brain injury?
9. What thought-related changes may occur due to a brain injury?
Shortened attention span
Memory problems
Poor judgment
Partial or complete loss of reading and writing skills
Problem-solving difficulties
Language problems, including communication deficits and loss of vocabulary
Inability to understand abstract concepts
Difficulty learning new things
10. What physical changes may occur due to a brain injury?
Weakness
Muscle coordination problems
Full or partial paralysis
Changes in sexual functioning
Changes in the senses (hearing, sight, touch, etc.)
Seizures (also called traumatic epilepsy)
Sleep problems
Speech difficulties
11. What subtle or severe personality and behavioral changes may occur due to a brain injury?
Difficulty with social skills
Inability to empathize with others
Tendency to be more self-centered
Inability to control one’s emotions
Increases in irritability and frustration
Inappropriate and/or aggressive behavior
Extreme mood swings
Depression (individuals with TBI are considered to be at a high risk for depression)
12. Why is it so difficult to predict the outcome of a TBI?
Although the field of neuroscience has advanced our understanding of TBI considerably, we still know a limited amount about the brain’s capacity to heal following injury. Instead of predicting outcomes, rehabilitation professionals often create treatment plans to help people achieve specific goals.
These plans must take into account the severity of injury, the amount of time (if any) spent in a minimally conscious state, and available resources. Neuropsychological evaluations test for areas of specific impairment, and can be of great assistance in understanding the severity of injury. Armed with that information, rehabilitation workers can then help people with TBI reach their goals through therapy and other efforts.
13. What is the process of treating a TBI?
As soon as the injury occurs, most people should receive care in a medical center that specializes in trauma care. If the examining doctor believes that the injury is a mild TBI, then the patient is typically evaluated and tested and possibly discharged with the appropriate recommendations for follow-up care. Patients are told to immediately report any worsening of symptoms.
In the case of moderate and severe TBI, individuals may transition into surgery, intensive care, acute care, or any combination of the three. Specialists at every stage of treatment should be available to recommend subsequent stages of treatment. Once the person is medically stable, helpful treatment options may include the following:
Acute rehabilitation programs
Post-acute rehabilitation centers
Sub-acute care through a skilled nursing facility
Long-term care/supervised living for slow-to-recover patients
Coma stimulation programs
Residential facilities that specialize in TBI
Outpatient rehabilitation
Day treatment programs
Neuropsychological Testing
Neurological medication management
Epilepsy treatment centers
Neurobehavioral management programs
In-home treatment provided by medical professionals
Some rehabilitation may last weeks or months, while others may last years. Programs and treatments will change as you or your loved one’s particular needs change. Some centers may also provide respite care services for family members who need to place their loved one into temporary care.
14. What are the differences among all the rehabilitation specialists who may be needed?
Neurologists: Neurologists are doctors who are trained in the diagnosis and treatment of nervous system disorders. These can include diseases of the brain, spinal cord, muscles, and nerves.
Physiatrists: Physiatrists are medical experts in rehabilitation medicine. They typically oversee the rehabilitation process.
Occupational, Physical, Speech and Language Therapists: These therapists work with a person with TBI to regain cognitive and communication skills, physical abilities, and behavioral skills.
Vocational Rehabilitation Experts: These experts are employment coaches who help with regaining job skills.
Behavioral analysts: These specialists create strategies for dealing with behavioral problems.
Neuropsychologists: These specialized psychologists focus on thinking skills and behavior problems.
Case managers/ care coordinators: Case managers/case coordinators assist people in finding and accessing needed programs and services.
Note: Some professionals also carry additional certification from the American Academy for the Certification of Brain Injury Specialists. See: http://www.aacbis.net/ for details.
15. Will I get better?
TBI is treatable, and treatment is always made better with the help of people who care about you. Keep in mind that TBI is considered a catastrophic injury; the greater the severity of the TBI, the less likely you are to return to your pre-injury physical and mental status.
There is a popular myth that suggests that there is a limited time frame for helping someone after a brain injury, but the fact is that many people continue to make gains in their recovery many years after the injury.
16. How long will it take to get better?
TBIs tend to heal slowly. In mild cases, symptoms may persist for weeks or months. For moderate to severe TBIs, some symptoms may resolve over the course of months or years, while others may persist for a lifetime.
17. How can I find financial assistance?
It takes a lot of money, time, and resources to deal with TBI effectively, so it’s no surprise that people with TBI and their families can be placed under tremendous financial strain. Financial assistance will vary based on the kind of TBI you have, the kind of insurance you carry, and even the state you live in. In many cases, those with TBI must make due with the few resources that are available.
Case managers or social workers may be available through treatment centers or through your state’s health and human services organizations. They may be aware of specific types of aid particular to your circumstances. Veterans, on the other hand, should approach their care coordinators to help identify options that may (or may not) exist.
18. What are some housing options for people with TBI?
Keeping and maintaining a home environment is difficult enough for the average person; with a TBI, housing issues can become a real problem. Finding help for your housing needs is a complicated, difficult task, and in some areas of the country, adequate housing simply may not be available.
Your local Department of Health may be able to direct you to housing assistance programs in your area. For those requiring in-home medical assistance, some programs may be available through local nursing homes, rehabilitation centers, or community support programs.
19. Will I be able to resume my old job, or find new, meaningful employment?
TBIs often upset a person’s ability to work, but many people who experience a TBI are able to return to their previous occupations. You may require additional assistance or certain technologies (voice recorders, organizers, or visual aids) in order to resume former duties, or you may enlist the help of a vocational rehabilitation expert to find new and meaningful employment. In severe cases, a person may not be able to physically participate in work.
20. Who will love me?
TBI does not affect your ability to love or be loved, but it can have an effect on relationships. While no studies offer information about relationships in the case of mild TBIs, one study reports that 46 percent of people who sustained moderate to severe TBI experienced a divorce within five years after their injury.
Despite the numbers affecting the severe TBI population, many people with TBI are able sustain and nurture their relationships with minimal difficulties. In some cases, leaning on resources such as support groups or relationship counselors can be a helpful way to deal with relationship challenges.
21. How do I deal with all these new emotions like depression, anxiety, anger?
Emotional hardship is one of the most common consequences of TBI. It is a frightening and frustrating injury, and can cause you to feel depressed, anxious, or angry. If emotional problems begin to have a direct effect on your ability to function and maintain your relationships, you should seek the help of a therapist or counselor familiar with TBI issues. Additionally, neuropsychiatrists and neuropsychologists may be of help in diagnosing and treating emotional disorders that arise after TBI.
Source: Michael Paul Mason, BrainLine – FAQ